In relation to the previous articles on the bones of the leg and the types of joints, we now analyze the joints of the leg (lower limb).
Knowing the joints of the leg is very important to have a detailed anatomical context of the lower body.
Joints of the leg that we are going to analyze
The joints of the leg (lower limb) are found at 3 levels according to their location (1, 2):
- Proximal – Hip.
- Intermediate – Knee.
- Distal – Ankle-foot.
Next, we will detail all these joints of the leg in a detailed manner.
Hip joint
The coxofemoral joint of the leg is the most proximal of the leg joints (1,2, 3,4,5).
It is a ball-and-socket type (3) and is a multiaxial spheroidal leg joint (1, 2, 4) whose main function is to provide stability (1) and support weight (1, 4). However, the hip can perform movements in all planes (3, 4):
- Flexion and extension.
- Abduction and adduction.
- Internal rotation and external rotation.
- Circumduction.
Thus, given its main functions, it is one of the most stable leg joints (1, 2, 4) but also one of the most mobile in the human body (2).
Articular surfaces
They are the femoral head (spherical) and the semilunar surface of the acetabulum with inferior concavity (1, 2, 4). Both articular surfaces are covered by hyaline cartilage (except for the fovea of the femoral head) (2, 4).
The acetabular labrum is inserted at the acetabular rim/border (1, 2, 5), increasing the articular area by almost 10% (2). Thus, more than half of the femoral head is within the acetabulum (2, 4), which provides much of the stability to the hip joint (4).
The acetabular labrum and the transverse acetabular ligament, which is an inferior continuation of the acetabular labrum (1, 4, 5), make the acetabulum a complete cavity (hole) (2, 4, 5).
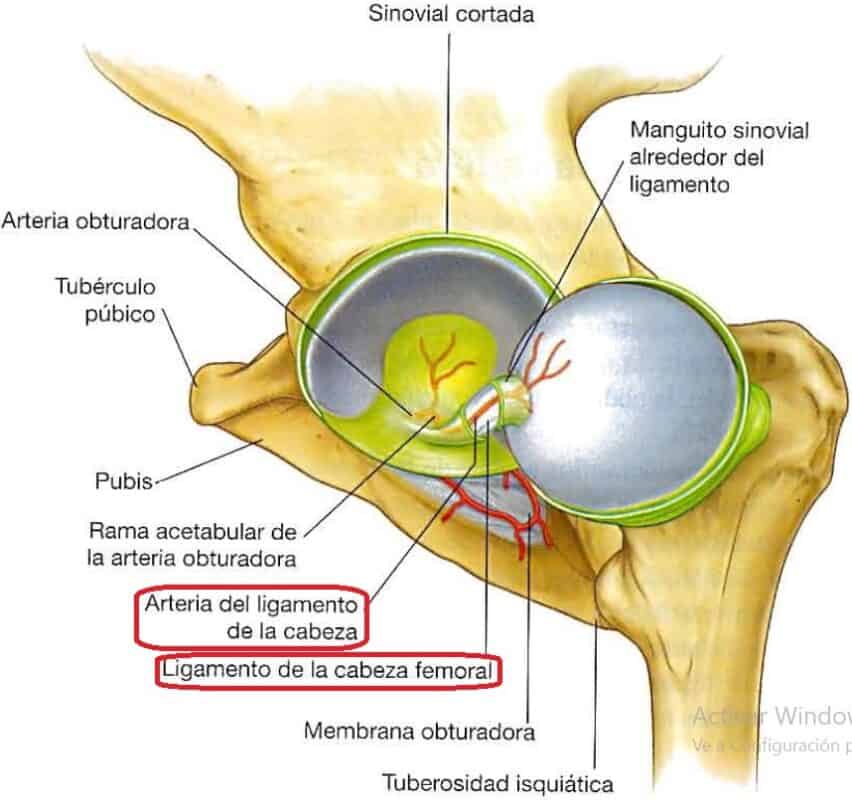
The part of the acetabular fossa not occupied by the ligament of the head of the femur is filled by a “fat pad” (2, 5) so that the entire bony surface within this leg joint is covered by soft tissue.
Union elements
The union elements of the hip joint are the articular capsule, the ligaments of the fibrous membrane, the ligament of the head of the femur (1, 2, 4), and the tendons of the rectus femoris and insertion of the psoas-iliacus (1).
Articular capsule
Resistant (2), tight in the middle (1), and formed by the internal synovial membrane and the external fibrous membrane.
Synovial membrane:
Covers the deep surface of the capsule (1, 2, 4). It has a fold that covers the ligament of the head of the femur and its artery (1, 4). It inserts at the edge of the articular surface of the femur, envelops the femoral neck, and folds proximally to insert into the articular surface of the acetabulum (4).
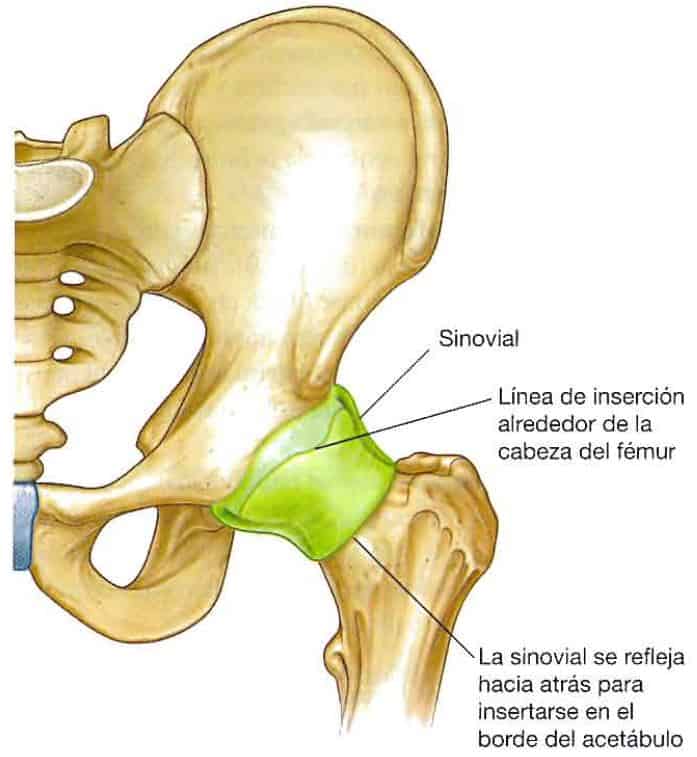
Fibrous membrane:
It is the outer layer of the articular capsule, strong, robust (4), and lax (2).
It originates around the acetabular cavity (including the transverse ligament) (2, 4), in part of the edge of the obturator foramen (4, 5), follows a helical path (2), and inserts along the intertrochanteric line of the anterior part of the femoral neck (2, 4, 5).

Ligaments
Within the leg joints, in the hip, we find 3 ligaments that reinforce the articular capsule and a deep ligament that connects the femoral head with the coxal acetabulum (1, 2, 3, 4, 5).
Ligaments of the articular capsule:
There are 3, and they are formed from the thick parts of the fibrous membrane (2), originating in the coxal and spiraling to the femur (2, 4, 5), reinforcing the articular capsule and providing stability to the hip joint (4).
Given their spiral orientation, they tighten in hip extension, compressing the articular capsule (1, 2, 4).
This reinforces the stability of the hip joint (2, 4) and requires less energy expenditure to maintain bipedalism (4), but reduces the extension range to 10-20º from the vertical (2).
The 3 ligaments originate around the acetabulum (1, 2, 4, 5), each in one of the embryonic bones of the coxal (1, 2, 4):
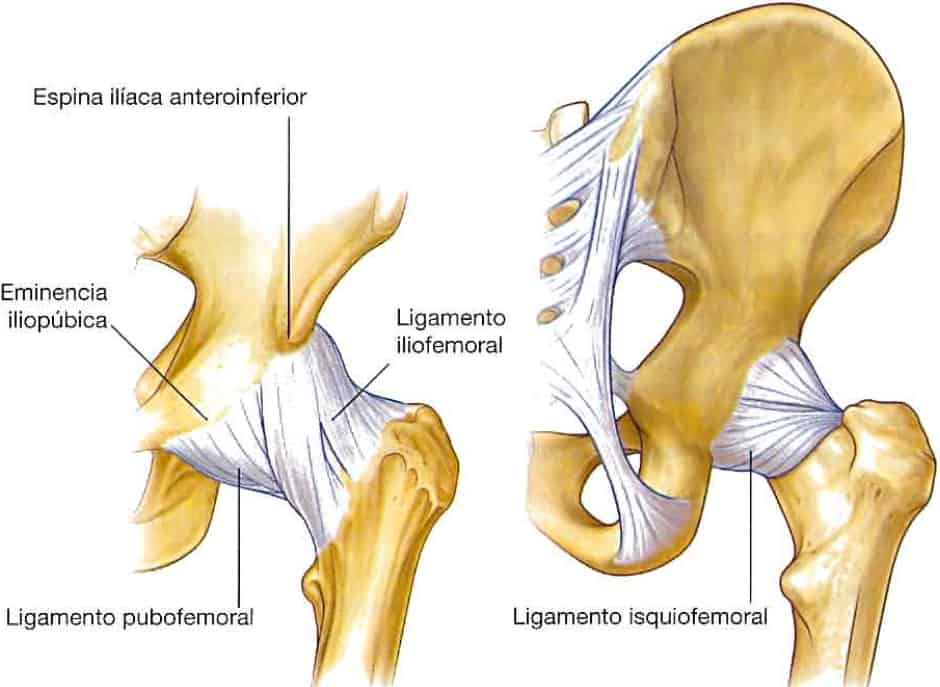
- Iliofemoral ligament:
Located at the anterosuperior level (2, 4, 5), it originates at the anteroinferior iliac spine and the acetabular rim and inserts along the intertrochanteric line (2, 4). It has an inverted “Y” shape (2, 4, 5) because the fibers at the ends of its insertion are thicker than the central ones (4). In bipedalism, it prevents the hip from hyperextending (2). - Pubofemoral ligament:
Located at the anteroinferior level (2, 4, 5), it originates at the obturator crest of the pubis (2, 5) and the iliopubic eminence (4, 5) and distally joins the fibrous membrane of the articular capsule and the inner part of the iliofemoral ligament (2, 4). It tightens in hip extension and abduction, preventing hyperabduction (2). - Ischiofemoral ligament:
Located at the posterior level, it originates at the acetabular rim of the ischium (2, 4, 5) and the ischial tuberosity (4, 5) and spirals to insert into the femoral neck (2, 5). It is the weakest of the 3 (2).
Ligament of the head of the femur:
It inserts into the fovea of the femoral head and the acetabular fossa (4), the transverse acetabular ligament, and the edges of the acetabular notch (2, 3, 4, 5). This ligament contains a branch of the obturator artery to supply the femoral head (2, 4).
Knee
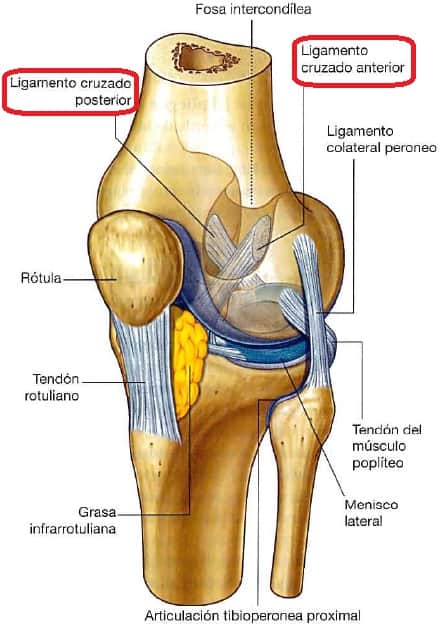
Of the leg joints, the knee is the first articular complex (from proximal to distal) (1, 2, 3, 4, 5) formed by 2 joints (1, 4, 5):
- Femoropatellar joint (or femoropatellar), involving the femur and the patella.
- Femorotibial joint (or tibiofemoral), involving the medial and lateral femoral condyles and their tibial counterparts.
On the other hand, it can be considered that there are independently an internal femorotibial joint and an external one, which would give a complex of 4 joints (2). Overall, the knee is the largest and most superficial synovial leg joint in the body (2, 4).
The femorotibial joint supports weight, and the femoropatellar joint serves as a pulley for the quadriceps tendon, protecting it from wear (4).
Of the leg joints, the femorotibial is a non-congruent joint (1, 2), making it mechanically weak (2), requiring significant reinforcement from ligaments, muscles, and tendons (1, 2), with muscles being the most important factor for its stability (2).
Articular surfaces
All the leg joints, the knee, are covered by hyaline cartilage, within the same articular cavity and the same articular capsule (2, 3, 4). They are as follows:
Femur:
There are 3 articular surfaces, 1 for the patella and 2 for the tibia (1, 2, 3, 4, 5).
- Patellar surface / trochlea / hinge (1, 4, 5) In this case, trochlea/hinge refers to the femoral surface that articulates with the patella (6). It has an inverted “V” shape and is the junction point of the femoral condyles (4, 5).
- Femoral condyles (one medial/internal and one lateral/external). The surface that articulates with the tibial condyles in extension is flatter than the one that articulates in the rest of the flexo-extension range (3, 4), so the position of greatest stability for the knee is full extension (2).
Patella or kneecap:
2 articular surfaces on the posterior surface, one medial/internal and one lateral/external (1, 4, 5).
Tibia:
2 tibial condyles, one medial/internal and one lateral/external. They are concave, and the 2 menisci are inserted into them (1, 2, 3, 4, 5).
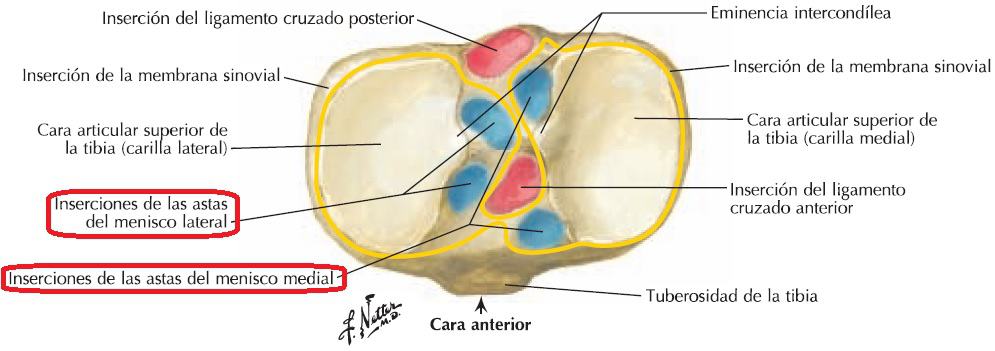
Menisci:
There are 2 menisci, one medial/internal and one lateral/external, one on each side of the intercondylar region (1, 2, 3, 4, 5) and connected to each other by their anterior edges thanks to the transverse ligament of the knee (2, 3, 4, 5).
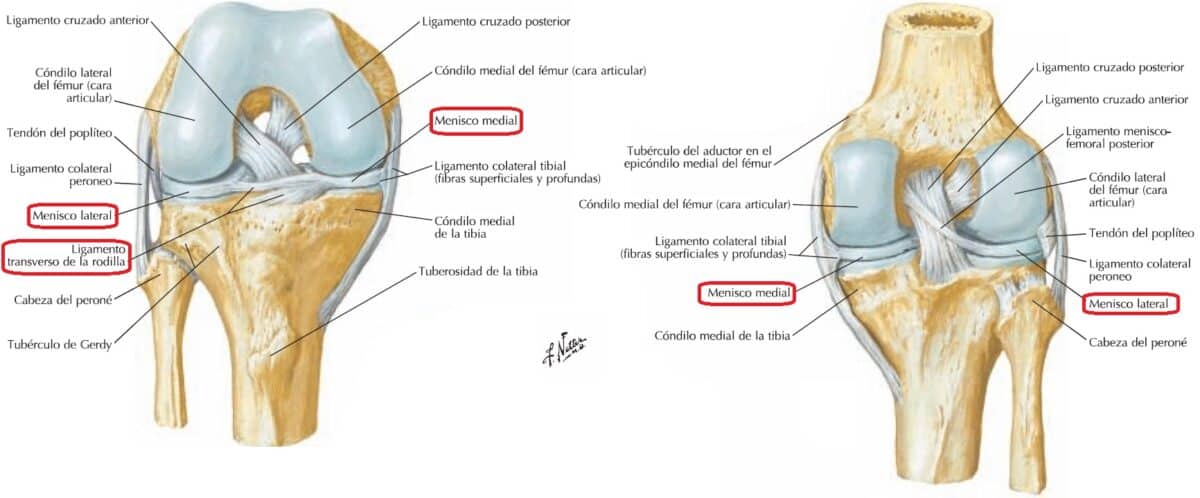
They are crescent-shaped fibrocartilages, the internal one longer and narrower, and the external one shorter and wider (1, 2).
They accommodate the femoral condyles on the tibial condyles, increasing the congruence of their articulation during movement and cushioning impacts (2, 4) thanks to their shape and their sliding on the tibial plateau to adapt to the movements of the femur and tibia (2, 3).
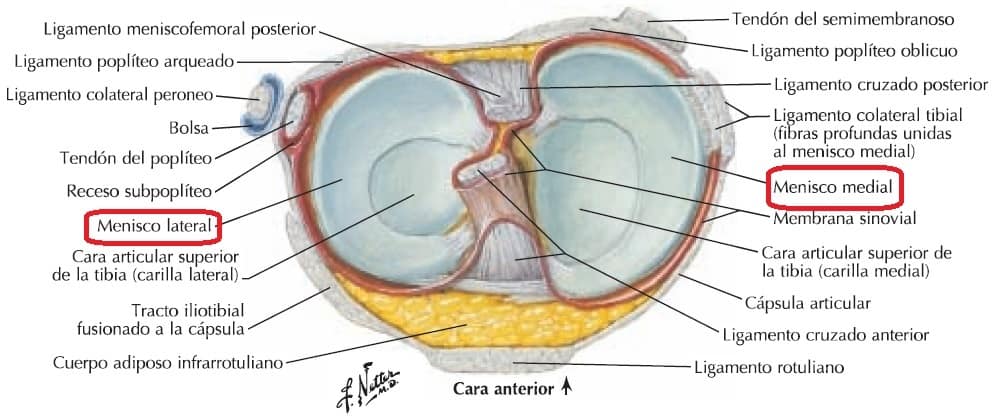
The menisci are firmly attached to the tibial condyles (1, 2), both inserted at each end/horn (anterior and posterior) to the corresponding facets of the intercondylar region of the tibial plateau (2, 4, 5).
The medial meniscus is attached by its outer edge to the articular capsule and the tibial collateral ligament, unlike the external meniscus (2, 3, 4), making the latter more mobile (2, 4).
The lateral meniscus, at the posterior level, is connected to the internal femoral condyle and the posterior cruciate ligament by the posterior meniscofemoral ligament (2).
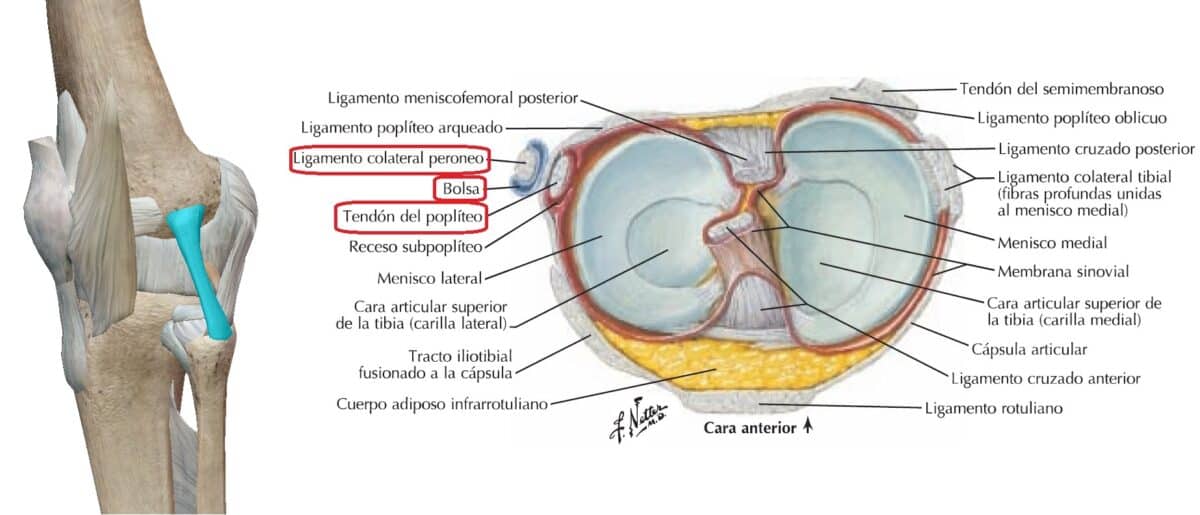
It is also connected to the tendon of the popliteus muscle (2, 4), one portion of which runs between the lateral meniscus and the fibular collateral ligament, and the other inserts into the posterior horn of the lateral meniscus (2).
Union elements
The union and passive stability of the knee articular complex are provided by the articular capsule, the synovial membrane, and a series of ligaments, some of which also serve as reinforcement for the articular capsule (2, 4).
Articular capsule
Formed by an internal synovial membrane and an external fibrous membrane (2, 4).
Synovial membrane:
Covers the deep part of the capsule (1, 2, 4) and all intracapsular structures not covered by cartilage (2), except for the central part (from anterior to posterior) where it presents a fold (infrapatellar synovial fold), isolating the cruciate ligaments and the infrapatellar fat pad (1, 2, 4).
It inserts at the edges of all the articular surfaces of the knee and at the edges of the 2 menisci.
On each side of the patellar ligament, 2 alar folds (internal and external) are formed, covering the infrapatellar adipose body internally on each side of the patellar ligament.
Additionally, the synovial membrane forms a series of bursae that reduce tendon friction during movements (2, 4):
- Suprapatellar bursa.
Superior to the patella, between the femur, the quadriceps muscle, and its tendon.
It inserts at its apex into the articular muscle of the knee. - Subpopliteal bursa/recess
Located on the posterior side of the knee, inferior to the lateral meniscus between the lateral condyle of the tibia and the tendon of the popliteus muscle.
Fibrous membrane:
It is thick in several parts, especially at the posterior level, to prevent recurvatum (1, 2), and incomplete (2). The thicker parts form the intrinsic ligaments (2).
It originates in the femur, around the articular surface of the femoral condyles, including the intercondylar fossa.
It inserts at the edge of the tibial plateau, except for the posterior edge of the lateral tibial condyle, where it forms an opening for the tendon of the popliteus muscle to pass through (2).
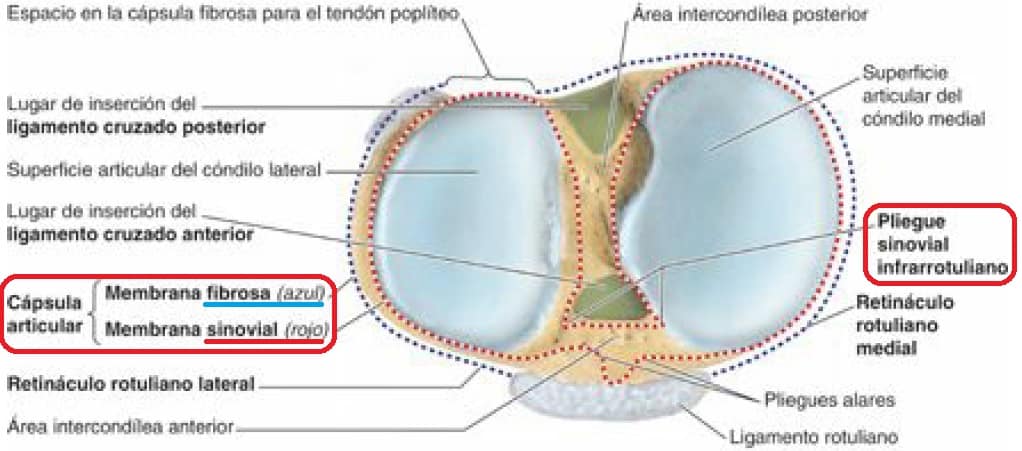
At the anterior level, the fibrous membrane follows the edges of the quadriceps tendon, the patella, and the patellar ligament, with these same structures being anterior to the fibrous membrane (2, 3, 5).
Ligaments
In the knee joint, there are intra-capsular ligaments and extra-capsular ligaments (2, 3, 4, 5).
Intra-articular ligaments
In addition to the menisci (2), they are the anterior cruciate ligament (ACL) and the posterior cruciate ligament (PCL) (2, 3, 4, 5). They are intracapsular and extrasynovial, connecting the femur and tibia (1, 2, 3, 4, 5) and serving as the central pivot of the knee (1, 2).
- Anterior Cruciate Ligament:
It inserts into one of the anterior articular facets of the intercondylar region of the tibia and the posterior part of the lateral wall of the femoral intercondylar fossa (2, 4, 5). Thus, its path is superior, posterior, and lateral (1, 2, 3, 4, 5).
Although it is weaker than the PCL (2), it is a strong ligament (1) that prevents anterior tibial translation relative to the femur (1, 2, 4), posterior femoral translation relative to the tibia (1, 2), and knee hyperextension (2). - Posterior Cruciate Ligament:
It inserts into the posterior and lateral part of the intercondylar region of the tibia and the medial wall of the femoral intercondylar fossa at its anterior part (1, 2, 4, 5). Thus, its path is superior, anterior, and medial (1, 2, 3, 4, 5).
It is stronger than the ACL (2) and prevents posterior tibial translation relative to the femur (1, 2, 4), anterior femoral translation relative to the tibia (1, 2), and knee hyperflexion (2). When the knee bears weight in flexion, it is the main passive stabilizer of the femur in the knee joint (2).
The PCL has better vascularization than the ACL (1), which is relatively scarce (2).
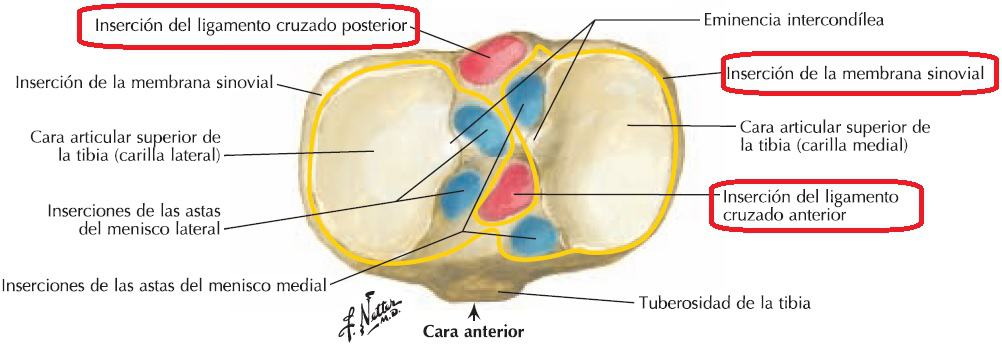
With all the above, the cruciate ligaments of the knee are located crossed in the sagittal and frontal planes (1, 2, 3, 4, 5), crossing the ACL laterally relative to the PCL (2, 3, 4, 5).
Additionally, since they have an oblique position, either one or part of one of them is always under tension (2).
Thus, given their arrangement, both ligaments twist around each other in internal rotation and untwist in external rotation (2), limiting internal rotation (1, 2) (to about 10º), while external rotation reaches almost 60º (if the knee is near 90º of flexion), with the tibial collateral ligament being responsible for limiting it (2).
Extra-capsular ligaments
The articular capsule is reinforced on its outer side by a series of intrinsic ligaments:
Patellar ligament:
Also called the patellar tendon, it is the inferior continuation of the quadriceps tendon and extends from the inferior edge of the patella to the tibial tuberosity (2, 3, 5, 7).
It is a strong ligament (2) that reinforces the articular capsule at the anterior level. On the sides are the patellar retinacula (medial and lateral) (2, 3, 5), which keep the patella aligned in the femoral trochlea and support the capsule on the sides of the patella (2).

Knee collateral ligaments:
These ligaments are located on each side of the knee (medial and lateral) (3, 4, 5). They tighten in extension and loosen as the knee flexes (1, 2), allowing and preventing rotation depending on the degree of flexion (2). There are 2:
- Superficial Medial Collateral Ligament:
It originates at the proximal and posterior part of the medial femoral epicondyle and inserts at the posteromedial edge of the tibia (proximal insertion) and the medial tibial surface (distal insertion) (4, 8, 9), through soft tissues (semimembranosus tendon-proximal; pes anserine bursa-distal) (8, 9). Depending on the knee position, its tibial insertions have more or less prominence (8, 10):- Proximal: main passive stabilizer of the knee in valgus.
- Distal: main passive stabilizer of the knee in external rotation and 30º flexion and main passive stabilizer (along with the posterior oblique ligament) in internal rotation.
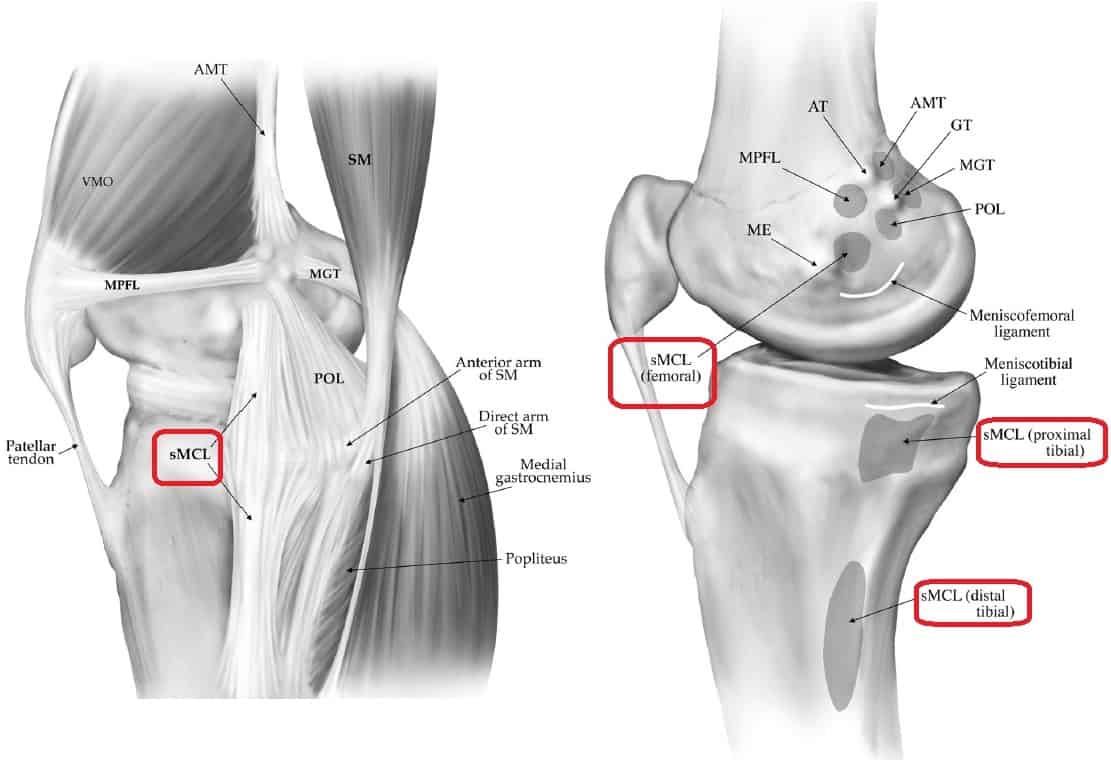
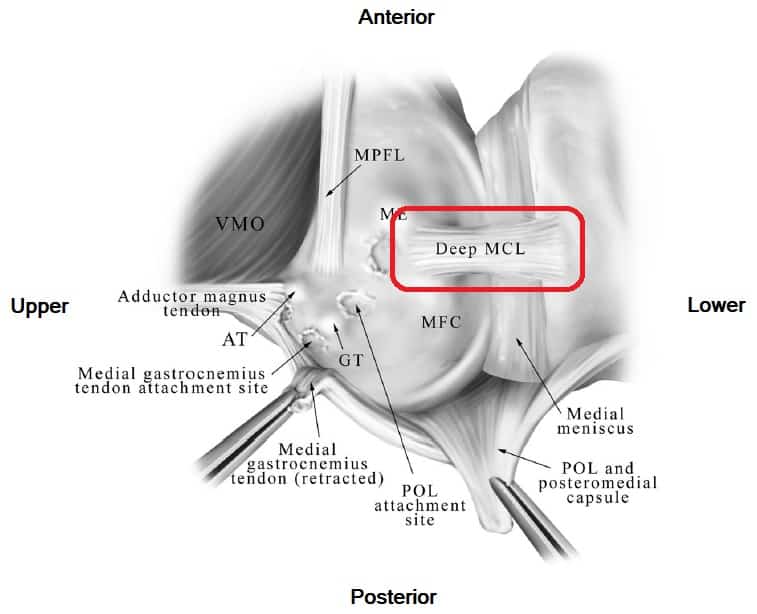
- The deep medial collateral ligament
Inferior to the superficial medial collateral ligament, it is related to the articular capsule (4, 8) and is attached to the internal meniscus (1, 2, 8, 9) through its femoromeniscal and tibiomeniscal bundles (1, 8, 9).- The femoromeniscal bundle originates inferior to the superficial medial collateral ligament on the femur (8).
- The tibiomeniscal bundle inserts inferior to the medial tibial plateau (8).
Fibular Collateral Ligament / Lateral/External Collateral Ligament:
It is a strong ligament (2) that originates at the lateral femoral epicondyle, superior to the origin of the popliteus muscle, and inserts on the external side of the fibula (1, 4, 2).
A bursa separates it from the fibrous membrane (4), and the popliteus tendon separates it from the external meniscus (2).
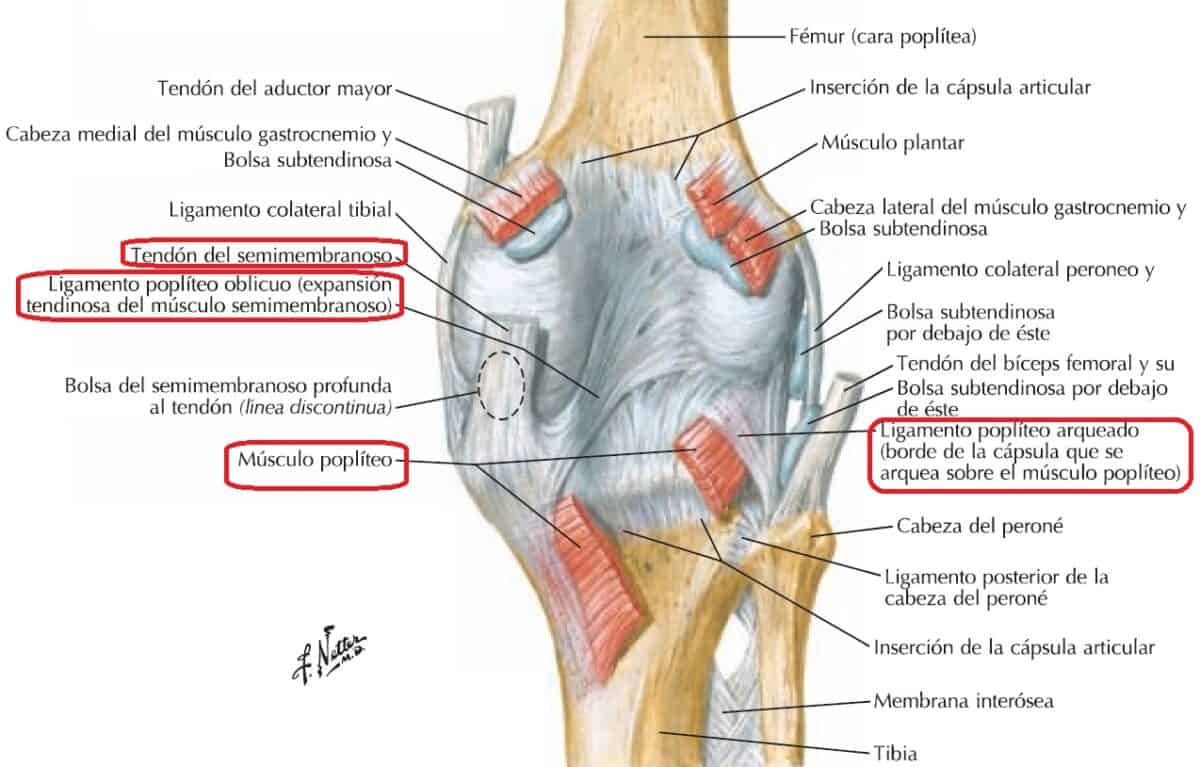
Oblique Popliteal Ligament:
It originates from the semimembranosus tendon at the medial tibial condyle and extends to the lateral femoral condyle, merging with the articular capsule at the posteromedial level (2, 5), reinforcing the articular capsule posteriorly (2).
Arcuate Popliteal Ligament:
It originates posteriorly at the fibular head, extends superomedially, arching over the popliteus tendon, and inserts into the fabella, a sesamoid bone of the external gastrocnemius tendon (2, 3, 5).
Ankle
Of the leg joints, the ankle is the second articular complex. It connects the leg and foot (1, 2, 3, 4, 5), and the tibia, fibula, and talus articulate in it (1, 2, 4, 5).
Therefore, the ankle consists of the inferior tibiofibular joint and the talocrural joint or talocrural (1, 2, 4, 5), but it should also include the superior tibiofibular joint due to its functional relationship with the inferior one (1).
Tibiofibular joints
There are 2, one superior (superior tibiofibular joint) and one inferior (tibiofibular syndesmosis or inferior tibiofibular joint) (1, 2). The movements of the superior tibiofibular joint depend on the movements of the tibiofibular syndesmosis (2).
Superior tibiofibular joint
Located in the knee region (1, 5) but due to its functional relationship with the inferior tibiofibular syndesmosis (1, 2), it can be considered part of the ankle (1).
It is a synovial leg joint that is connected to the knee region by the fibular collateral ligament (1, 2, 4, 5), but it has its own articular capsule (1, 2).
Articular surfaces
There are 2 articular surfaces, 1 for each bone of the joint (1, 2, 4).
Tibia:
Fibular articular facet below the lateral tibial condyle. It is located at the posterolateral level (1, 2).
Fibula:
Articular facet located on the fibular head (2, 4) at the superointernal level (4).
Both surfaces are flat (1, 4) and circular in shape (4).
Union elements
The union elements of the superior tibiofibular joint are the articular capsule, which contains a synovial membrane, and 2 ligaments (1, 2).
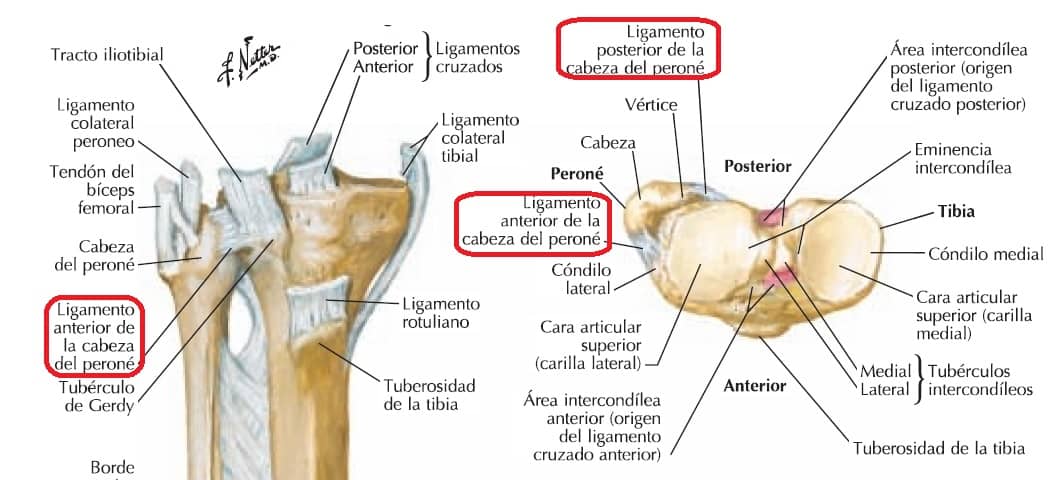
The articular capsule is tense and inserts at the edges of the articular surfaces, reinforced by the anterior ligament of the fibular head and the posterior ligament of the fibular head (2, 4).
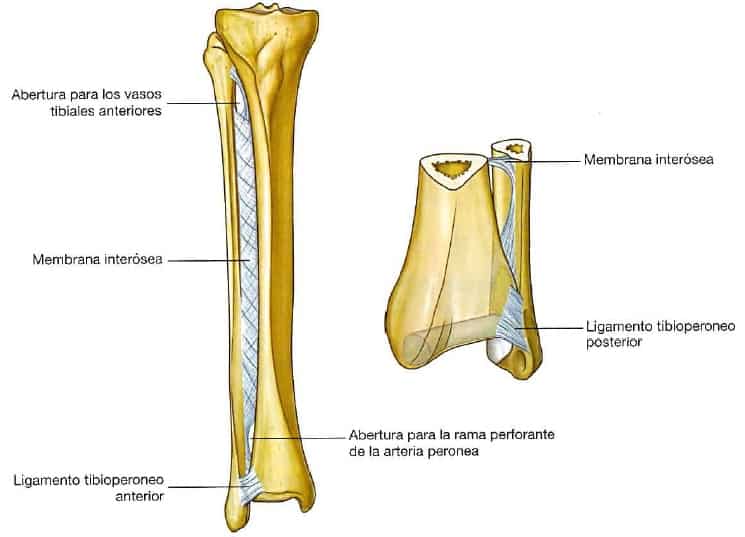
Tibiofibular syndesmosis
The tibiofibular syndesmosis is the fibrous joint between the distal ends of the tibia and fibula (1, 2, 4).
Articular surfaces
The articular surfaces are the internal triangular facet of the distal end of the fibula and the fibular notch of the tibia, also triangular, located laterally at the distal end of the tibia (2, 4).
They approximate or separate during the flexion-extension of the talocrural joint, facilitating the fit of the talus (1, 2).
Union elements
The union elements are a series of ligaments that connect the distal ends of the tibia and fibula, reinforcing their joint (1).
Anterior tibiofibular ligament and posterior tibiofibular ligament:
They are strong ligaments (2) that consolidate the joint (2, 4).
From the anterolateral (anterior tibiofibular ligament) and posterolateral (posterior tibiofibular ligament) parts, they extend inferiorly and laterally to insert into the distal end of the fibula (4).
The posterior tibiofibular ligament continues at a deep and distal level, forming the inferior transverse tibiofibular ligament, firmly connecting the medial tibial malleolus and the lateral fibular malleolus (2).
Interosseous tibiofibular ligament:
It is a strong ligament, the most important of the tibiofibular syndesmosis. It extends superiorly into the interosseous membrane (2).
Interosseous membrane:
As indicated, it is an extension of the interosseous tibiofibular ligament (2) and connects the tibia and fibula by their respective diaphyses (2, 4, 5). It inserts into the lateral interosseous edge of the tibia and the medial interosseous edge of the fibula (2, 3, 4, 5).
Its fibers are oriented inferolaterally, allowing the fibula to ascend (1) and limiting its descent (2). In the upper and lower parts of the interosseous membrane, there are 2 openings that serve as passages for blood vessels (2, 4).
On the other hand, in addition to firmly connecting the tibia and fibula, the interosseous membrane serves as a surface for muscle insertion (1, 2, 4, 5).
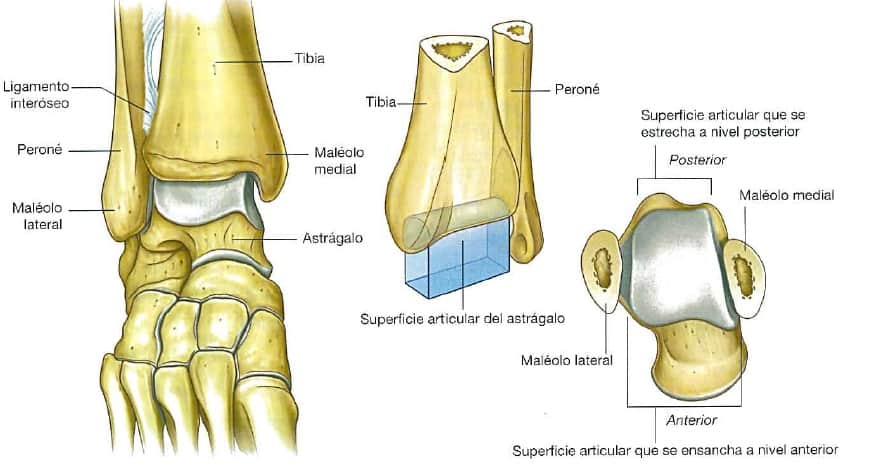
Talocrural joint
It is the synovial joint (1, 2, 4) between the distal ends of the tibia and fibula with the talus (1, 2, 4, 5). It performs abduction-adduction and inversion and eversion movements (2), but mainly performs flexion-extension movements (2, 4).
Articular surfaces
All the bony articular surfaces of the ankle are covered by hyaline cartilage (1, 2, 4). They are (1, 2, 4, 5):
Tibia:
- The inferior surface of the distal end.
- The external surface of the internal malleolus.
Fibula:
- Internal surface of the external malleolus
Talus:
- The trochlea of the talus, in which there are 3 differentiated surfaces (2, 4, 5, ):
- Superior, it is the trochlea of the talus. It articulates with the inferior end of the tibia.
- Internal, it articulates with the internal malleolus.
- External, it articulates with the external malleolus.
The articular surfaces of the tibia and fibula (2, 4) and part of the posterior tibiofibular ligament (2) form a hollow, the malleolar mortise, in which the dome of the talus fits (2, 4).
Thus, they form a trochlea (1, 2) of variable separation (1) because the talus is wider in its anterior part than in the posterior part. This makes it somewhat more unstable in dorsal extension and more stable in dorsal flexion (2, 4).
Union elements
The union elements are the articular capsule, which contains a synovial membrane, and a series of ligaments (1, 2, 4, 5), some of which have already been described.
Articular capsule
It inserts around the articular surfaces, at a deep level it is covered by a synovial membrane, and at a superficial level, the fibrous membrane is reinforced by ligaments (2, 4).
Synovial membrane:
It inserts at the edges of the articular surfaces (4), is lax (2), and covers the fibrous membrane internally (2, 4).
Fibrous membrane:
It inserts at the edges of the articular surfaces (2, 4), is thin at the anterior and posterior levels, and is reinforced at the internal and external levels by the medial and lateral collateral ligaments respectively (2).
Ligaments
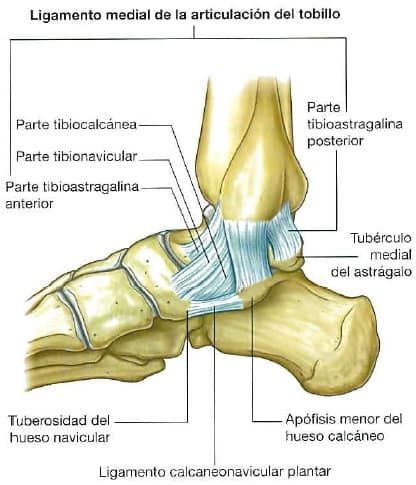
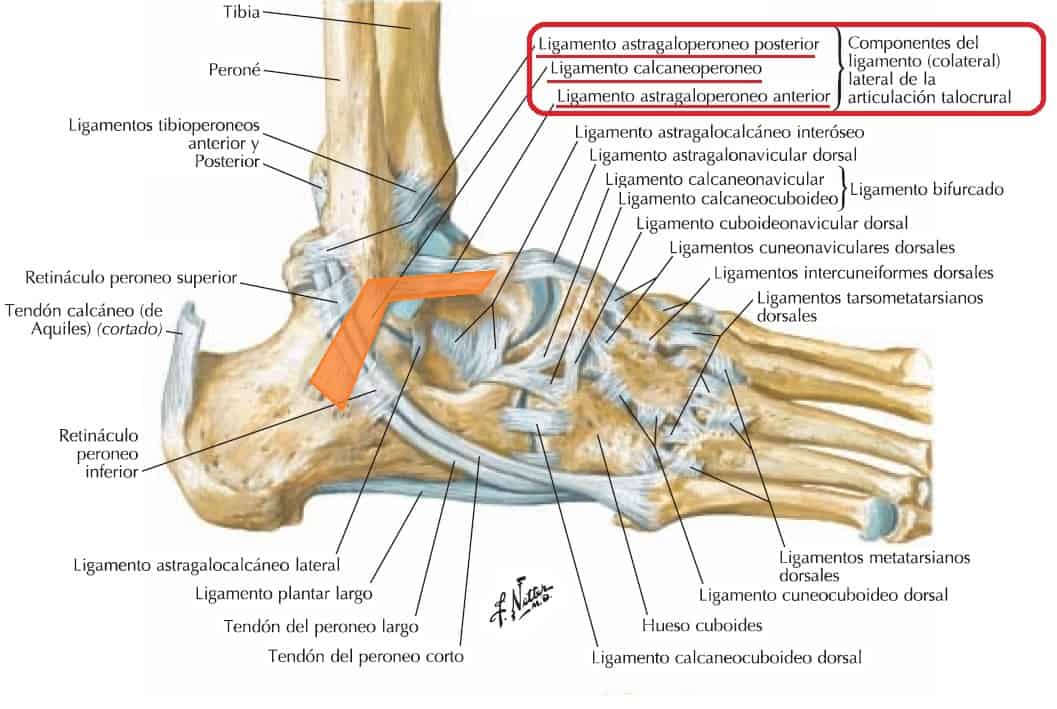
The talocrural joint and its capsule are reinforced by 2 ligaments, the medial collateral ligament and the lateral collateral ligament (1, 2, 3, 4, 5).
Medial collateral ligament:
Also called the deltoid ligament (2, 4). It is strong and has 4 bundles, which give it a fan shape (2, 4, 5). It has a single point of origin on the internal malleolus, and each bundle inserts at a different point, with contiguous insertions (2, 4, 5):
- The tibionavicular bundle inserts anterior to the navicular tuberosity and part of the plantar calcaneonavicular ligament.
- The tibiocalcaneal bundle inserts into the sustentaculum tali.
- The anterior tibiotalar bundle, deeper, inserts into the internal surface of the talus.
- The posterior tibiotalar bundle inserts at 2 points on the talus, on the internal surface and the internal tubercle.
Lateral collateral ligament:
It is a ligament complex traditionally described as consisting of 3 separate ligaments with different orientations (1, 2; 4, 5):
- The anterior talofibular ligament, weak, flat, and with an anterointernal path. It originates at the anterior edge of the lateral malleolus and inserts into the neck of the talus.
- The posterior talofibular ligament, thick, strong, and with a posterointernal path. It originates in the malleolar fossa and inserts into the lateral tubercle of the posterior process of the talus.
- The calcaneofibular ligament originates at the anterior apex of the lateral malleolus, extends posteroinferiorly, and inserts into the lateral surface of the calcaneus.
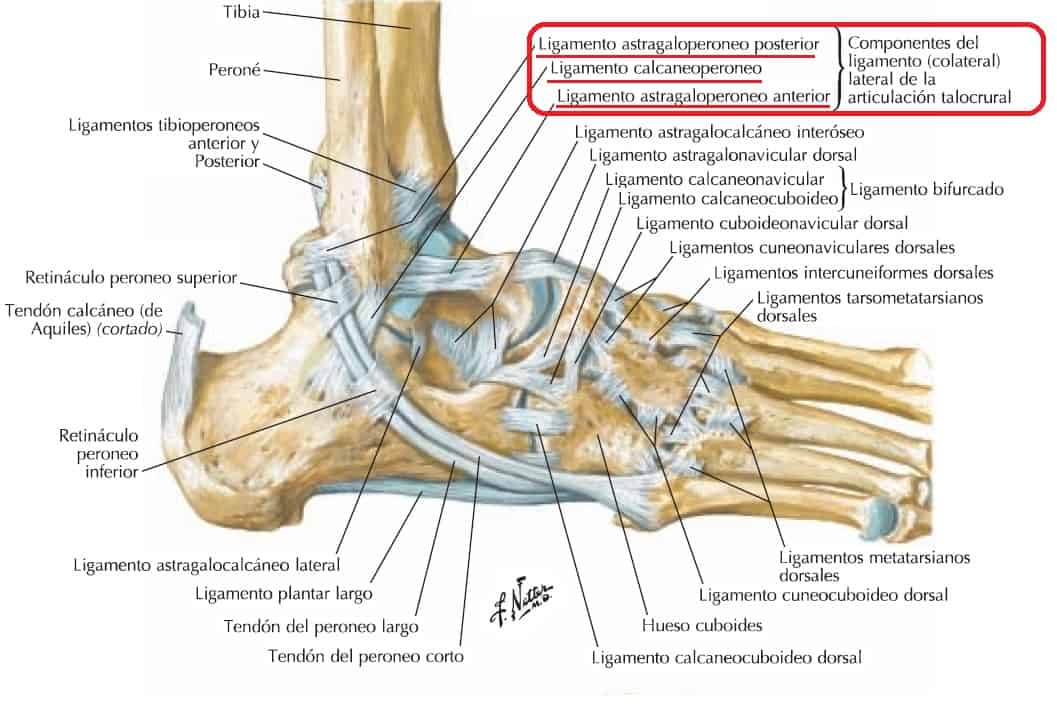
However, Vega et al (2018) (11) found that the 2 bundles of the anterior talofibular ligament (superior and inferior) are different anatomical and functional structures, separated from each other, with different points of origin and insertion (the inferior bundle just below the superior bundle) and the superior bundle being intraarticular and the inferior bundle extraarticular.
Additionally, they found that the inferior bundle is connected to the calcaneofibular ligament through arch-shaped ligamentous fibers, forming what they called (11, 12).
Foot
The foot contains the largest number of leg joints (1, 2, 3, 4, 5) and is the connection of the body with the ground, which is why, to adapt to its characteristics, the foot presents several interlines (transverse tarsal joint and tarsometatarsal joint) (4, 5).
These interlines divide the foot into the hindfoot (talus and calcaneus bones and adjacent soft tissues), midfoot (navicular, cuboid, and cuneiform bones and adjacent soft tissues), and forefoot (metatarsal bones, and phalanges and adjacent soft tissues) (13, 14, 15).
The hindfoot and midfoot form the tarsus, and the metatarsus and phalanges form the forefoot. Therefore, the metatarsus connects the tarsus with the phalanges (2). However, sometimes the foot is described in only 2 parts, the hindfoot, which would encompass the tarsus, and the forefoot, which would encompass the metatarsus and phalanges (as well as the corresponding soft tissues of each part of the foot) (1, 2).
Thus, the interline that divides the foot into hindfoot (tarsus) and forefoot is the tarsometatarsal joint (5, 15, 16).
Tarsal joints
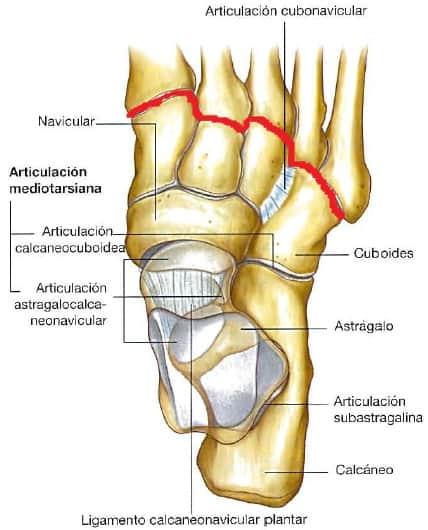
The tarsus is a functional articular complex that encompasses several joints (1, 2, 5):
- Subtalar joint.
- Transverse tarsal joint.
- Talocalcaneonavicular joint.
- Calcaneocuboid joint.
- Intercuneiform joints.
- Cuneonavicular joint.
Subtalar joint
Although sometimes the same term is used to encompass the talocalcaneal joints and the talocalcaneonavicular joints (2), the subtalar joint is a trochoid synovial joint (17) formed by the talus and the calcaneus (1, 2, 4) and is involved in the inversion and eversion movements of the foot (2, 4).
Articular surfaces
The articular surfaces, both of the talus and the calcaneus, are located at the posterior level (2, 4):
Talus:
Posterior articular surface for the calcaneus (2, 3, 4) with a concave shape (2, 3).
Calcaneus:
Posterior articular surface for the talus (2, 3, 4, 5) with a convex shape (2, 5).
Union elements
It has a weak articular capsule that contains a synovial membrane (1, 2) as well as a series of ligaments that fix and stabilize these leg joints (1, 2, 4, 5).
The articular capsule is reinforced by (1, 2, 4):
- Internal talocalcaneal ligament.
- External talocalcaneal ligament.
- Posterior talocalcaneal ligament.
- Interosseous talocalcaneal ligament.
Transverse tarsal joint
Formerly known as Chopart’s joint or amputation (1, 3), it separates the hindfoot from the midfoot (13, 14). It is formed by 2 separate joints (1, 2) but functionally interdependent (1) and form the first interline of the foot (2, 5).
The transverse tarsal joint favors the inversion and eversion movements of the subtalar joint, serving as a pivot for the midfoot and forefoot over the hindfoot (2, 4).
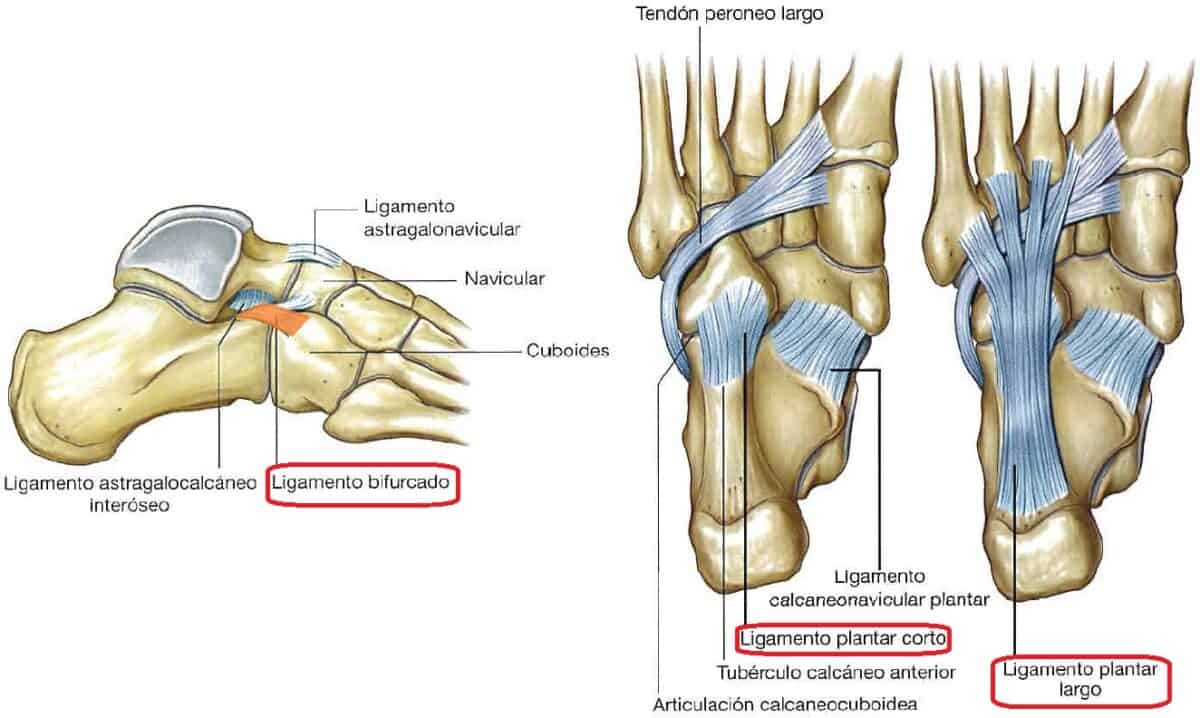
Of the leg joints that form the transverse tarsal joint are the talocalcaneonavicular joint (the talonavicular part) and the calcaneocuboid joint (1, 2, 4, 5), which are connected by the 2 bundles of the bifurcated ligament (1, 5).
This ligament originates in the anterior and superior part of the calcaneus and divides into the calcaneocuboid ligament and the calcaneonavicular ligament (4, 5).
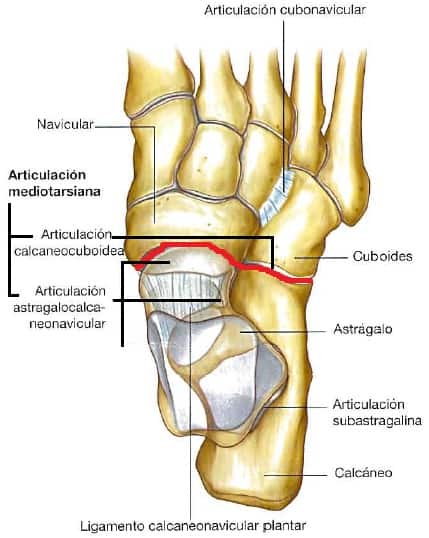
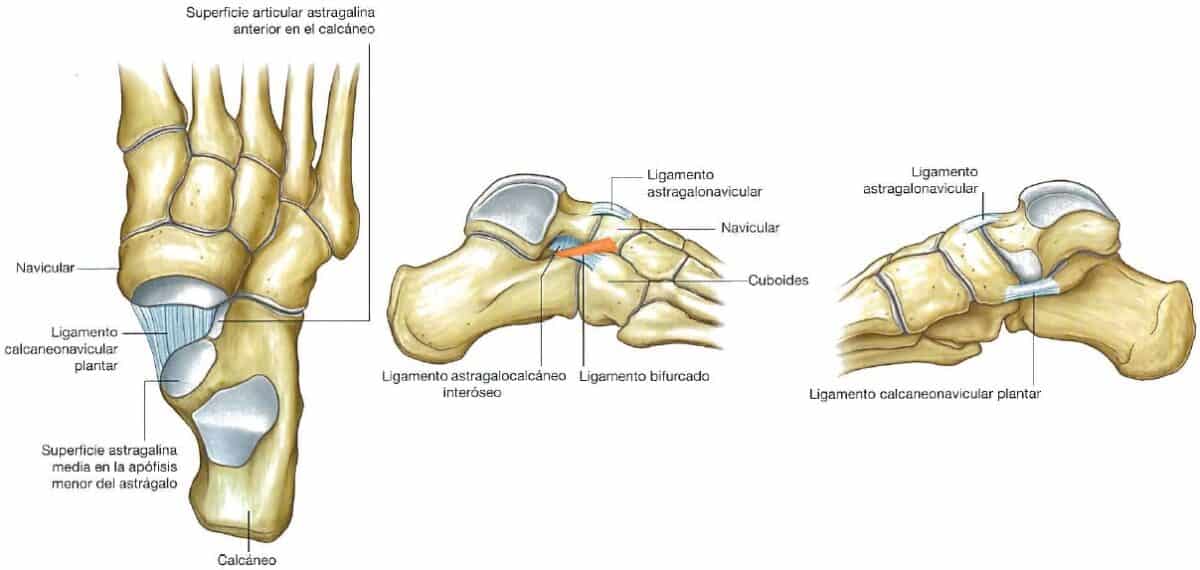
Talocalcaneonavicular joint
Of the leg joints, it is the internal joint of the transverse tarsal joint. It is a synovial joint (1, 4) spheroidal (1, 2) between the talus, calcaneus, and navicular bones (1, 2, 4) and the plantar calcaneonavicular ligament (4).
Articular surfaces
The articular surfaces of the talocalcaneonavicular leg joints are: (1, 4, 3, 5):
Talus:
- Anterior articular facet for the calcaneus on the inferior surface of the talar head (for the calcaneus).
- Medial articular facet on the inferior surface of the talar head (for the calcaneus and plantar calcaneonavicular ligament).
- Head of the talus (for the navicular).
Calcaneus:
- Anterior facet on the superior surface.
- Medial facet of the sustentaculum tali.
Both are for the talus.
Plantar calcaneonavicular ligament:
- Superior edge (for the talus).
Navicular:
- The concave surface of the navicular (for the talus).
Union elements
The talocalcaneonavicular leg joint is protected by the articular capsule and its synovial membrane, and a series of ligaments (1, 2).
The articular capsule partially protects these leg joints (2), and several ligaments reinforce it (1, 2, 4) at the posterior, superior, and inferior levels (4):
Plantar calcaneonavicular ligament:
Reinforces the articular capsule at its inferior part. It is a thick, wide ligament (4), and its deep surface is covered with cartilage (1). It originates at the sustentaculum tali and inserts into the posterior surface of the navicular (2, 4, 5).
It supports the head of the talus (2, 4), is involved in weight transfer from this bone (2), and participates in the passive maintenance of the longitudinal arch of the foot (2, 4).
Interosseous talocalcaneal ligament:
Located in the tarsal sinus, reinforcing the articular capsule at its posterior part (4). It has 2 bundles (1), is very strong (1, 2), and separates the subtalar joint from the talocalcaneonavicular joint (2).
Talonavicular ligament:
Reinforces the articular capsule at the superior level. It originates at the tarsal neck and inserts into the superior surface of the navicular (3, 4, 5).
Calcaneonavicular ligament:
It is the internal portion of the bifurcated ligament. Its insertion in the navicular bone occurs on the supero-external surface of the navicular (4, 5).
Calcaneocuboid joint
Of the leg joints, it is the joint of the calcaneus and cuboid bones and is the lateral joint of the transverse tarsal joint (1, 2, 4, 5).
It is a synovial leg joint (1, 4) of the saddle type (1).
Articular surfaces
The articular surfaces are (2, 3, 4, 5):
Calcaneus:
- Anterior articular facet.
Cuboid:
- Posterior articular facet.
Union elements
The calcaneocuboid leg joint has its own synovial articular capsule (1, 2, 4). Additionally, a series of ligaments also reinforce the joint (1, 2, 4).
Calcaneocuboid ligament:
It is the lateral portion of the bifurcated ligament. Its insertion in the cuboid bone occurs on the supero-internal surface (4, 5).
Plantar calcaneocuboid ligament:
Also called the short plantar ligament (2, 5), it is superior to the long plantar ligament (2, 3, 4, 5).
It is a short, wide (4), and strong ligament (1, 4) that originates at the anterior tubercle of the calcaneus and inserts into the inferior surface of the cuboid (2, 3, 4). This ligament supports the calcaneocuboid leg joint and contributes to the passive maintenance of the external plantar arch (2, 4).
Long plantar ligament:
It is the longest plantar ligament and is inferior to the short plantar ligament (4, 5).
It originates between the anterior tubercle and the tuberosity of the plantar surface of the calcaneus and inserts into the cuboid groove for the peroneus longus tendon, except for its superficial fibers, which extend to the metatarsal bones (2, 4) 2nd, 3rd, 4th, and 5th (2, 4, 5).
Prior to its insertion into the metatarsal bases, it forms a “tunnel” for the peroneus longus muscle (2, 4, 5). It is the strongest ligament involved in the passive maintenance of the external plantar arch (2, 4).
Cuneonavicular joint
It is one of the leg joints located between the navicular bone and the cuneiform bones (1, 2, 4).
Articular surfaces
The articular surfaces are (2, 3):
Navicular:
- Articular facets for the cuneiform bones (1st, 2nd, and 3rd).
Cuneiforms:
- Posterior surface of each of the cuneiform bones.
Union elements
The joint between these 4 bones has a common articular capsule, reinforced by the dorsal and plantar cuneonavicular ligaments (2, 5).
Tarsometatarsal joints
These leg joints form the second interline of the foot and separate the tarsus from the forefoot (2, 3, 5), which was known as Lisfranc’s joint/amputation (1, 3).
They are small leg joints (2) flat (16) between the distal tarsal bones (cuboid and 3 cuneiforms) and the proximal ends of the metatarsal bones (1, 2, 3, 4, 5, 16).
These leg joints together perform slight sliding movements (2, 4) and are involved along with the transverse tarsal joint in pronation-supination (4).
On the other hand, the 1st tarsometatarsal leg joint performs flexion-extension and rotation movements (4).
Articular surfaces
The articular surfaces correspond proximally to the cuneiform bones and the cuboid and distally to the 5 metatarsal bones (1, 2, 3, 4, 5).
Cuneiforms (3, 5):
- Anterior articular surfaces for the respective metatarsals.
Cuboid (3, 5):
- Anterior articular surface for metatarsals IV and V.
Metatarsals (I-V) (1, 2):
- Metatarsal bases.
Union elements
The tarsometatarsal leg joints are reinforced by independent articular capsules (2) and by plantar, dorsal (1, 2, 5), and interosseous ligaments (2, 5).
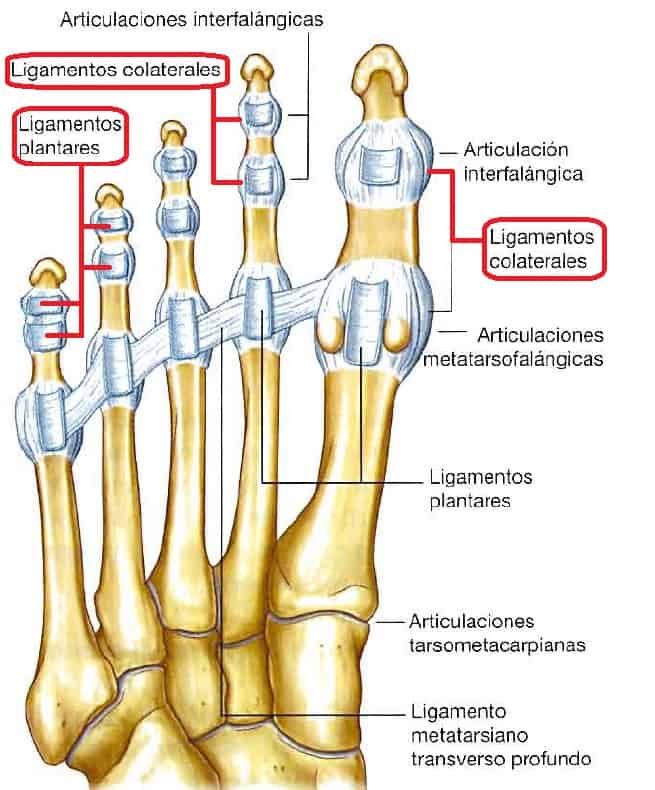
Forefoot joints
The leg joints, specifically of the forefoot, connect the 5 metatarsal bones to each other, these to the respective phalanges, and the phalanges of each toe to each other (1 joint for the first toe and 2 for the others) (1, 2, 3, 4, 5).
Intermetatarsal joints
These leg joints are synovial flat joints (2) that connect the proximal end of each metatarsal to the proximal end of the adjacent metatarsal, except for the first (2, 3, 4, 5).
Therefore, the fifth metatarsal has a single intermetatarsal joint, while the II, III, and IV metatarsals have 2, one internal and one external (2, 3, 4, 5).
Articular surfaces
The articular surfaces are located on the sides of the proximal end of each metatarsal (the fifth on the internal side) (2, 3, 4, 5).
Union elements
Each intermetatarsal leg joint has its own articular capsule (2). Also, a series of ligaments reinforce the 4 external intermetatarsal joints (2, 3, 5):
- Dorsal intermetatarsal ligaments.
- Plantar intermetatarsal ligaments.
- A plantar intermetatarsal ligament connects metatarsals I and II (5).
- Interosseous intermetatarsal ligaments.
Metatarsophalangeal joints
The metatarsophalangeal leg joints are the joints between each of the metatarsal bones and the corresponding proximal phalanx (2, 3, 4, 5).
They are synovial ellipsoid joints (1, 2, 4) that primarily perform flexion-extension movements, but also abduction-adduction, internal-external rotation, and circumduction (2, 4).
Articular surfaces
The articular surfaces of the leg joints are the distal ends of each metatarsal and the proximal end of the corresponding proximal phalanx (2, 3, 4, 5).
Under the plantar surface of the distal end of the first metatarsal, there are 2 sesamoid bones, one medial and one lateral. They are connected to the first phalanx by the tendon of the short flexor muscle of the first toe, which has a medial and a lateral head (1, 3, 4, 5).
Union elements
Each leg joint of this type has its own synovial articular capsule, reinforced by an internal collateral ligament and an external collateral ligament (1, 2, 3, 4, 5).
At the plantar level, each capsule is reinforced by a plantar ligament that creates a groove for the tendons of the long flexor of the first toe (in the first metatarsophalangeal leg joint, between the 2 sesamoid bones) and the tendons of the short flexor of the toes and long flexor of the toes (metatarsophalangeal joints II-V) (3, 4, 5).
On the other hand, the deep transverse metatarsal ligaments (there are 4) connect the distal ends of the metatarsals to each other (3, 4, 5), making the 5 toes function as a unit (4).
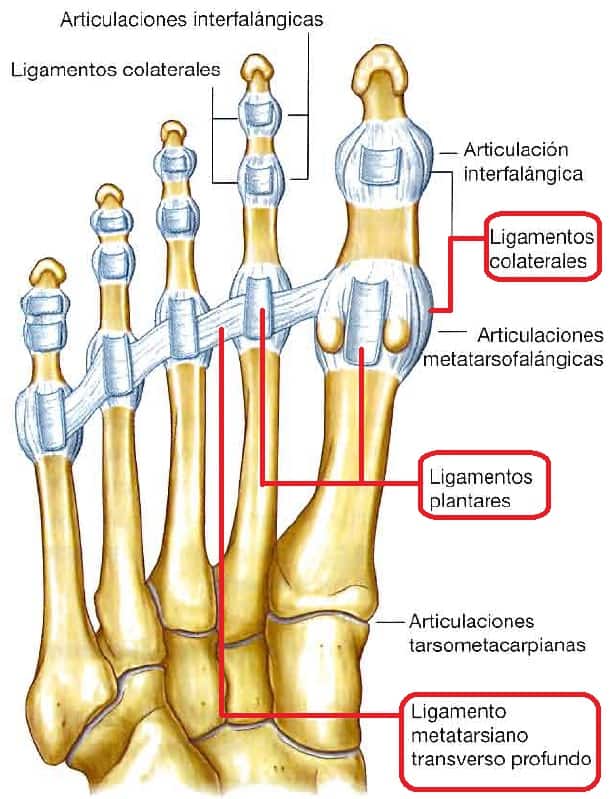
Interphalangeal joints
They are the most distal leg joints (1, 2, 3, 4). They are synovial joints (1, 2) of the trochlear type (1, 2, 4) between the distal end of a proximal phalanx and the proximal end of the corresponding distal phalanx (1, 2, 3, 4, 5).
Each toe has a proximal interphalangeal joint and a distal one, except for the first toe, which has only one (1, 2, 3, 4, 5).
Articular surfaces
The articular surfaces are located on the distal ends (head of the proximal phalanges), proximal and distal (base and head of the intermediate phalanges), and proximal (base of the distal phalanges) of each phalanx (2, 3, 4, 5).
Union elements
Each interphalangeal leg joint is reinforced with its own synovial articular capsule (1, 2), by collateral ligaments (one internal and one external) (1, 2, 3, 4, 5), and by a plantar ligament (1, 2, 4).
As in the metatarsophalangeal leg joints, these plantar ligaments create a groove for (4):
- Tendon of the long flexor muscle of the first toe (interphalangeal leg joint of the first toe).
- Tendons of the short flexor of the toes and long flexor of the toes (interphalangeal leg joints of toes II-V).
Interactive game to learn the bones of the human body
Below we leave you an activity to interact and easily locate the main bones of the human body. Let’s see how many you get right!
Conclusions
The joints of the leg (lower limb) are found at 3 levels according to their location (1, 2):
- Proximal – Hip.
- Intermediate – Knee.
- Distal – Ankle-foot.
The joints of the leg are primarily designed to support the weight of the body (1). This is why the leg joints, a powerful passive stabilizing system.
On the other hand, although this article has tried to describe the arthrological characteristics of the leg joints exhaustively, the fact of describing all the leg joints has meant that many points of their description have had to be summarized.
In this article, we have conducted a detailed analysis of the leg joints, seeking to establish an anatomical context of our lower body.
Within the leg joints, there are many different types, and we hope this article is helpful to you.
Bibliographic references
- Dufour M.. (2012). Anatomy of the lower limb. EMC – Podiatry; 14(4), 1-12 [article E – 27-005-A-10]. https://doi.org/10.1016/s1762-827x(12)61929-4
- Moore K.L., Dailey A.F., Agur A.M.R. (2013). Clinically Oriented Anatomy: Leg Joints. 7th edition. Barcelona: Wolters Kluwer/Lippincott Williams & Wilkins Health.
- Staubesand J. (1991). Sobotta. Atlas of Human Anatomy. Volume 2. Thorax, Abdomen, Pelvis, and Lower Limb. 19th edition. Madrid: Médica Panamericana.
- Drake R.L., Vogl W., Mitchell A.W.M. (2005) Gray’s Anatomy for Students. 1st edition. Madrid: Elsevier Spain.
- Netter F.H.. (2011). Atlas of Anatomy. 5th edition. Barcelona: Elsevier (Masson publication). leg joints
- Real Academia Nacional de Medicina de España. (2012) Dictionary of Medical Terms. Femoral trochlea. Madrid, Spain: Médica Panamericana. Real Academia Nacional de Medicina de España. Dictionary of Medical Terms. Retrieved from: https://dtme.ranm.es/buscador.aspx?NIVEL_BUS=3&LEMA_BUS=troclea%20femoral. Accessed on 06/04/2021.
- Real Academia Nacional de Medicina de España. (2012) Dictionary of Medical Terms. Patellar tendon. Madrid, Spain: Médica Panamericana. Real Academia Nacional de Medicina de España. Dictionary of Medical Terms. Retrieved from: https://dtme.ranm.es/buscador.aspx?NIVEL_BUS=3&LEMA_BUS=TENDON%20ROTULIANO. Accessed on 06/04/2021.
- Barrera Oro, F.D. (2012). Reconstruction of the Medial Collateral Ligament and the Posterior Oblique Ligament in Chronic Knee Instability, leg joints. Arthroscopy. Virtual Publication, 19(3), 140-148.
- LaPrade, R. F., Engebretsen, A. H., Ly, T. V., Johansen, S., Wentorf, F. A., & Engebretsen, L. (2007). The anatomy of the medial part of the knee. The Journal of bone and joint surgery. American volume, 89(9), 2000–2010. https://doi.org/10.2106/JBJS.F.01176
- Griffith, C.J., LaPrade, R.F., Johansen, S., Armitage, B., Wijdicks, C., Engebretsen, L. (2009). Medial knee injury: Part 1, static function of the individual components of the main medial knee structures. The American journal of sports medicine, 37(9), 1762–1770. https://doi.org/10.1177/0363546509333852
- Vega, J., Malagelada, F., Manzanares-Céspedes, M.C., Dalmau-Pastor, M. (2018). The lateral fibulotalocalcaneal ligament complex: an ankle stabilizing isometric structure. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA, 28(1), 8–17. https://doi.org/10.1007/s00167-018-5188-8
- Real Academia Nacional de Medicina de España. (2012) Dictionary of Medical Terms. Arciform. Madrid, Spain: Médica Panamericana. Real Academia Nacional de Medicina de España. Dictionary of Medical Terms. Retrieved from: https://dtme.ranm.es/buscador.aspx?NIVEL_BUS=3&LEMA_BUS=arciforme. Accessed on 06/04/2021.
- Real Academia Nacional de Medicina de España. (2012) Dictionary of Medical Terms. Hindfoot. Madrid, Spain: Médica Panamericana. Real Academia Nacional de Medicina de España. Dictionary of Medical Terms. Retrieved from: https://dtme.ranm.es/buscador.aspx?NIVEL_BUS=3&LEMA_BUS=retropie. Accessed on 06/04/2021.
- Real Academia Española (2021) Real Academia Española: Dictionary of the Spanish Language. Midfoot. Madrid, Spain: Dictionary of the Spanish Language: https://dle.rae.es/mediopi%C3%A9. Accessed on 06/04/2020.
- Real Academia Nacional de Medicina de España. (2012) Dictionary of Medical Terms. Forefoot. Madrid, Spain: Médica Panamericana. Real Academia Nacional de Medicina de España. Dictionary of Medical Terms. Retrieved from: https://dtme.ranm.es/buscador.aspx?NIVEL_BUS=3&LEMA_BUS=antepie. Accessed on 06/04/2021.
- Real Academia Nacional de Medicina de España. (2012) Dictionary of Medical Terms. Tarsometatarsal joint. Madrid, Spain: Médica Panamericana. Real Academia Nacional de Medicina de España. Dictionary of Medical Terms. Retrieved from: https://dtme.ranm.es/busc